Table of Contents
Understanding the Process and Benefits of Soft Tissue Valve Replacement
Soft tissue valve replacement, also known as biological or bioprosthetic valve replacement, is a surgical procedure that involves replacing a damaged or diseased heart valve with a valve made from animal tissue. This procedure is a significant advancement in the field of cardiovascular surgery, offering a range of benefits to patients suffering from heart valve diseases.
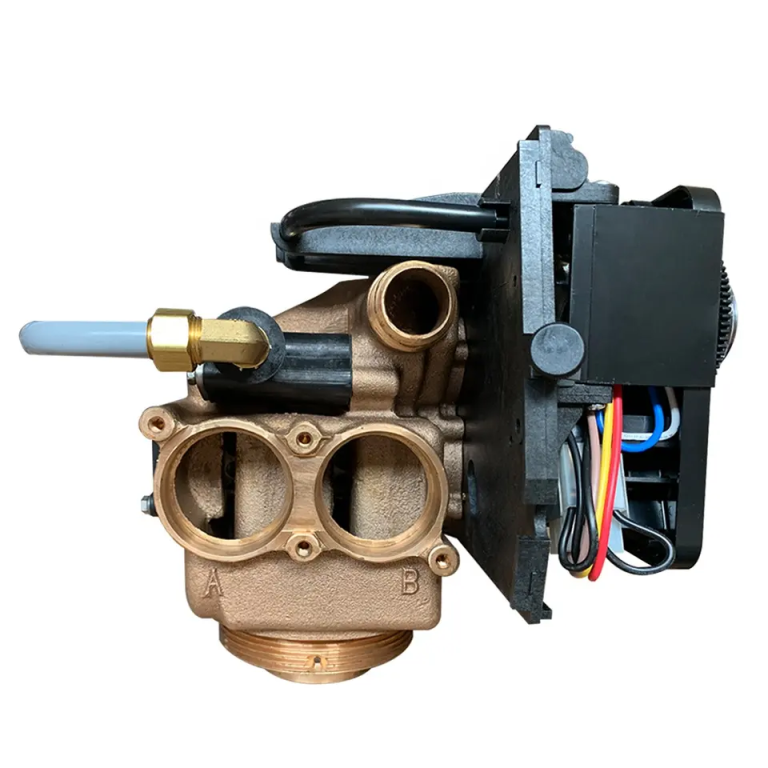
| Model | Central tube | Drain | Brine tank connector | Base | Maximum power | Operating temperature |
| 9500 | 1.9″(1.5″) O.D. | 1″NPTF | 3/8″& 1/2″ | 4″-8UN | 8.9W | 1℃-43℃ |
The human heart consists of four valves that control the flow of blood in and out of the heart. These valves can become damaged or diseased due to various reasons, including congenital defects, infections, or age-related degeneration. When this happens, the affected valve may not open or close properly, leading to a disruption in the blood flow. This can cause symptoms such as shortness of breath, chest pain, fatigue, and in severe cases, heart failure.
Traditionally, heart valve replacement has been performed using mechanical valves made from materials like metal or plastic. While these valves are durable and long-lasting, they come with a significant drawback: patients who receive them must take blood-thinning medications for the rest of their lives to prevent blood clots from forming on the valve. This requirement can be burdensome and carries its own risks, including a higher chance of bleeding complications.
| Model | Category | Water Capacity m3/h | LCD | LED | ICON | DIODE |
| CV-2 | Automatic Drain Valve | 0.5 |
Soft tissue valve replacement offers an alternative to mechanical valves. In this procedure, the surgeon replaces the damaged or diseased valve with a valve made from animal tissue, usually from a pig or cow. These tissue valves, also known as bioprosthetic valves, are treated to remove any cellular material that could cause an immune response, leaving behind a durable, flexible structure that can function much like a natural heart valve.
One of the main advantages of soft tissue valve replacement is that it typically does not require long-term use of blood-thinning medications. This can significantly improve the quality of life for patients, particularly those who are older or have other medical conditions that make taking these medications risky.
Another benefit of soft tissue valve replacement is that it can provide a more natural feel and function than mechanical valves. Patients often report that they can no longer hear the clicking sound that is characteristic of mechanical valves, and many find that their energy levels and overall well-being improve after the procedure.
However, it’s important to note that soft tissue valves may not last as long as mechanical valves. They tend to wear out over time, and may need to be replaced after 10 to 20 years, depending on the patient’s age and overall health. For this reason, soft tissue valve replacement is often recommended for older patients, or those who are not good candidates for long-term use of blood-thinning medications.
In conclusion, soft tissue valve replacement is a significant advancement in the treatment of heart valve diseases. It offers a range of benefits, including a reduced need for blood-thinning medications and a more natural feel and function. However, like all medical procedures, it also has its risks and limitations, and the decision to undergo this procedure should be made in consultation with a qualified healthcare provider. With the right information and guidance, patients can make an informed decision that best suits their individual health needs and lifestyle.
Exploring the Latest Advances in Soft Tissue Valve Replacement Techniques
Soft tissue valve replacement, a critical procedure in the field of cardiovascular surgery, has seen significant advancements in recent years. These advancements have not only improved the success rate of the procedure but also enhanced the quality of life for patients suffering from heart valve diseases. This article aims to explore the latest advances in soft tissue valve replacement techniques, shedding light on how these innovations are revolutionizing cardiovascular healthcare.
Traditionally, heart valve replacement has been performed using mechanical valves made from materials like titanium and carbon. While these valves are durable, they require patients to take blood-thinning medications for the rest of their lives to prevent blood clots. This necessity has led to the development and refinement of soft tissue valve replacements, also known as bioprosthetic valves. These valves, typically made from animal tissue, offer a more natural alternative and eliminate the need for lifelong anticoagulation therapy.
One of the most significant advancements in soft tissue valve replacement is the development of transcatheter aortic valve replacement (TAVR). This minimally invasive procedure allows surgeons to replace the aortic valve without opening the chest or stopping the heart. Instead, a catheter is used to guide the new valve to the heart through a small incision in the leg. This technique has proven to be a game-changer, particularly for high-risk patients who may not be suitable candidates for traditional open-heart surgery.

Another noteworthy development is the advent of sutureless and rapid deployment valves. These innovative valves are designed to reduce the complexity and duration of the procedure, thereby minimizing the risk of complications. The valves are pre-assembled and can be implanted quickly, reducing the time the patient spends on a heart-lung machine. This advancement has significantly improved patient outcomes, particularly in older patients and those with multiple comorbidities.
In addition to these procedural advancements, there have also been significant strides in the materials used for soft tissue valve replacements. For instance, the use of treated bovine pericardium or porcine heart valves has become increasingly common. These tissues undergo a series of treatments to enhance their durability and resistance to calcification, thereby extending the lifespan of the valve.

Moreover, the field of tissue engineering is making promising strides towards creating bioengineered heart valves. These valves, grown from the patient’s own cells, could potentially eliminate the risk of rejection and the need for immunosuppressive drugs. While still in the experimental stages, this technology holds immense potential for the future of soft tissue valve replacement.
In conclusion, the field of soft tissue valve replacement has seen remarkable advancements in recent years. From minimally invasive procedures like TAVR to the development of sutureless and rapid deployment valves, these innovations are making valve replacement safer and more effective. Furthermore, advancements in the materials used for these valves, as well as promising developments in tissue engineering, are paving the way for a future where heart valve replacement is less invasive, more durable, and tailored to the individual patient’s needs. As research continues and technology advances, we can expect to see even more improvements in this critical area of cardiovascular healthcare.